Reduced Pain of heavy A/R and backlog
for a pain management client

Our client a pain management practice in Northern Jersey switched RCM to us after identifying problems with their cashflows. After a free practice audit following were the
After deploying our team to first understand the problem and then correct the process and reduce the billing and A/R backlog. In the next 2 months, these were
Challenges Identified
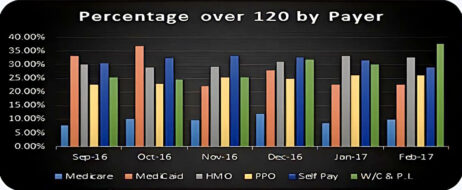
- A/R 20% at >120 days
- Incorrect filing of claims (invalid identification numbers, incorrect modifiers, and without prior authorization)
- Delayed filing of claims with 2 m in pending claims
- Compliance risk and insufficient documentation
- Denials resubmitted at a delay without proper corrections
Results Achieved
- A/R 20% at >120 days
- Increased monthly revenue by 25000
- Made billing cycle to current with zero pending claims at 48 hrs of receipt
- Reached operational metrics of 24 hrs for claim submission and 24-48hrs for payment posting
- Denial correction and re submission with 15 days
- Weekly dashboards and summaries for KPIs
Process improvement for multi-specialty
clients led to accelerated cash flow
One of the biggest practice Management companies based out in Southern California, US providing End to End RCM services.
Client’s Requirement
Our client is a practice management company serving over 50 physicians in 8 specialties. We were brought in to identify causes of revenue leakage
Challenges
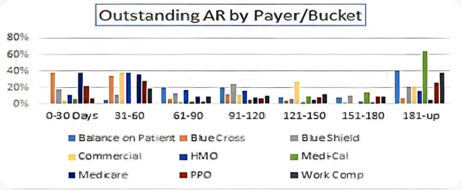
We identified that the database was highly unreliable with several issues:
- Payer data is heavy on HMOs and IPAs with a lot of individual provider contracts.
- The payer class is not correctly set up on practice management software.
- Delayed and duplicate claim submission.


Physician and Hospital Metrics
- Aged AR as a % of total outstanding and billed AR
- Net days in AR
- Total charge lag days
- Percent of patient schedule occupied
- Practice cash collection percentage
- Professional services denial
- Point-of-Service (POS) collection rate
- Primary/Specialty physician practice operating margin ratio
- Days in total discharged Not Final Billed (DNFB
- Bad debt
- Charity as a %age of uncompensated care
- Cost to collect by functional area
- Case Mix Index
Client Benefits
- Identified revenue bottlenecks
- Reduced revenue leakage by setting up required contracts in EMR
- Managing reimbursement trends with targeted follow ups
- Reduced bad debt by working on root cause analysis provided
- Accelerated cash flow across the enterprise
- Benchmark analysis for industry focused growth
